Trauma survivors endure much more than the initial event. Even after they’ve left the epicentre of harm, trauma lingers—deeply embedded in both the mind and the body. It isn’t just about what happened; it’s also about how the body continues to react long after the danger has passed.
Many people associate trauma only with large-scale tragedies—natural disasters, war, sexual violence, or severe childhood abuse. However, trauma can also stem from situations that are often minimised: relationship breakups, family estrangement, toxic workplaces, sudden losses, chronic illness, accidents, or witnessing distressing events. The common denominator is that the person felt overwhelmed, helpless, or emotionally unsafe.
The Hidden Toll of Trauma
One of the most misunderstood aspects of trauma is that survivors don’t simply “get over it.” They may not even be consciously thinking about the traumatic event, yet their nervous system continues to react as if the danger is still present. This can result in lasting psychological struggles like PTSD, anxiety, depression, or somatic symptoms (physical pain with no medical cause).
Often, people focus on fighting the symptoms—panic, numbness, rage, withdrawal—without recognising that these are not flaws or signs of weakness. They are survival responses hardwired into the body. And to understand them better, we need to look at the biology behind trauma.
Trauma and the Nervous System: Why We Freeze, Flee, or Fight
When someone experiences trauma, their reactions may seem confusing, not only to others but also to themselves. They might ask:
“Why did I go numb?”
“Why couldn’t I speak up?”
“Why did I lash out at someone I love?”
To answer these questions, we need to look beyond behaviour and into the body’s internal operating system—specifically, the autonomic nervous system.
The Polyvagal Theory: A Scientific Lens on Trauma
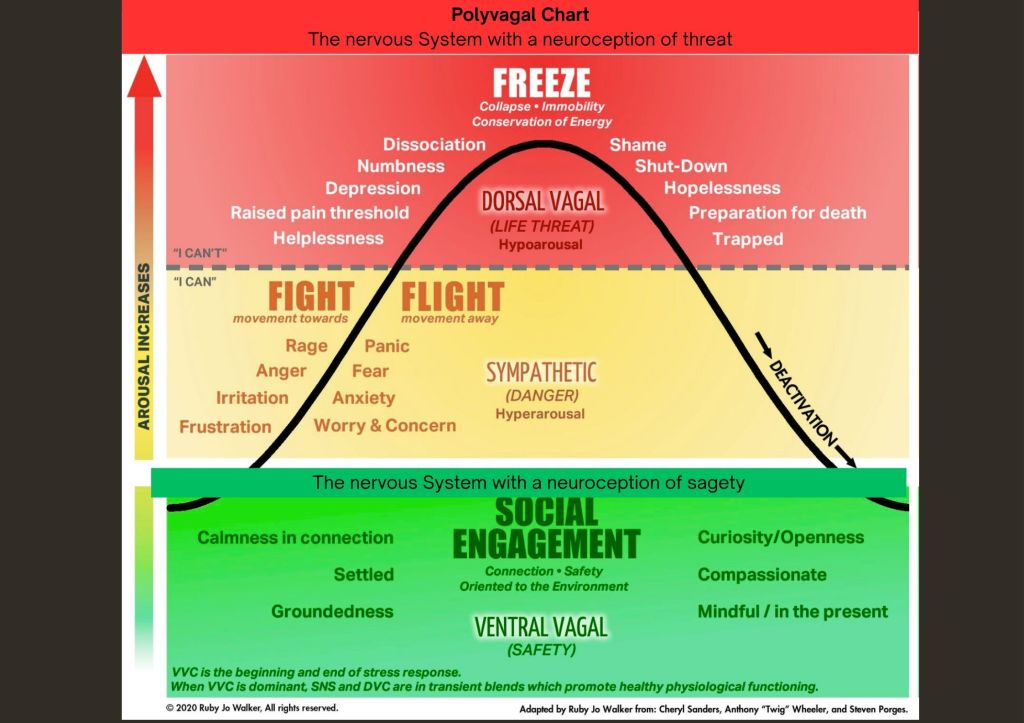
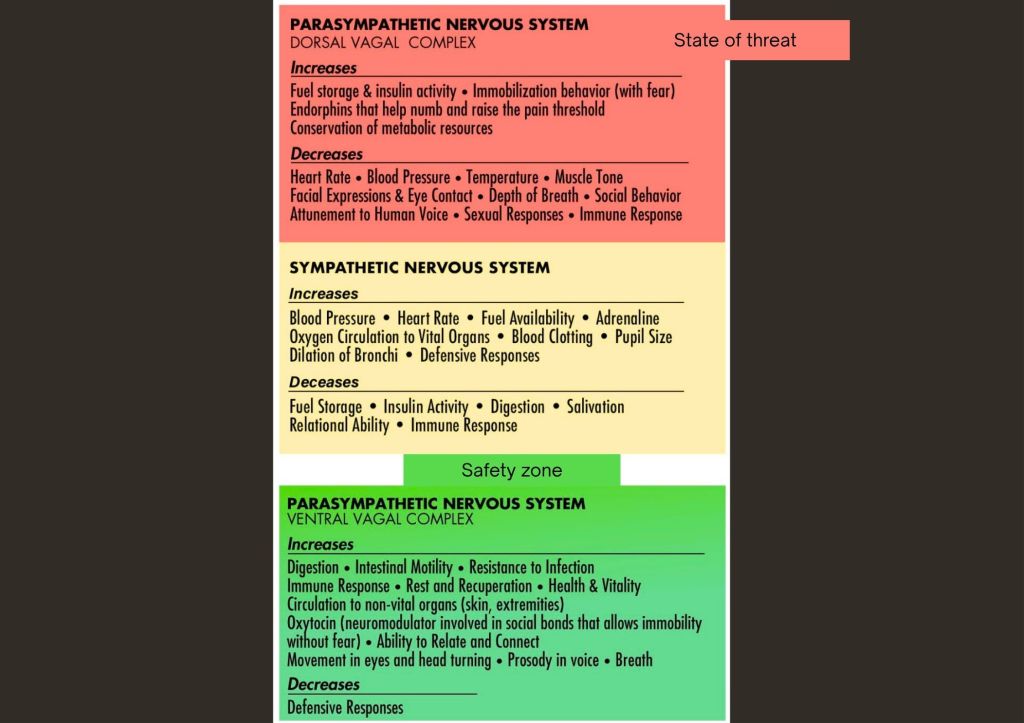
Developed by Dr. Stephen Porges, Polyvagal Theory offers a compassionate and science-backed way of understanding how trauma shapes our physiological states. According to this theory, the autonomic nervous system has three main pathways, and trauma shifts our ability to move fluidly between them.
Think of it as an “autonomic ladder”—we climb up and down these states depending on whether we feel safe or threatened.
1. Ventral Vagal State — Safety and Connection
This is the ideal state. In the ventral vagal state, we feel:
- Safe
- Calm
- Present
- Curious
- Connected to others
Here, we can process thoughts clearly, enjoy relationships, and regulate our emotions. For trauma survivors, however, accessing this state can be challenging. Even minor stressors can be perceived as danger, preventing them from feeling grounded or secure.
2. Sympathetic State — Fight or Flight
When the brain detects a threat, the body activates the sympathetic nervous system to prepare for survival.
Fight response may appear as:
- Anger or rage
- Yelling, aggression
- Defensiveness
- Flight response may manifest as:
- Anxiety or panic
- Avoidance
- Overthinking
- Restlessness or overworking
These reactions are not conscious choices. They’re automatic signals from the nervous system that say, “I’m not safe. I have to survive.”
Many trauma survivors become chronically stuck in this high-alert state, feeling constantly overwhelmed, irritable, or anxious—even when no real threat exists.
3. Dorsal Vagal State — Freeze or Shutdown
When fighting or fleeing isn’t an option, the body shifts into the dorsal vagal state. This is the freeze response—characterised by emotional numbing, collapse, or complete shutdown.
People in this state may say:
- “I can’t move.”
- “I feel nothing.”
- “I’m dead inside.”
- This response is especially common in:
- Childhood trauma
- Long-term neglect or abuse
- Situations where one had no escape
It’s the body’s way of saying: “I’m overwhelmed. I’ll survive by shutting down.” While it may have helped in the moment, staying stuck here can lead to long-term disconnection from oneself and others.
Trauma = Getting Stuck in Survival Mode
In a healthy nervous system, we move between states—activation and relaxation—based on the environment. This flexibility is essential for emotional balance.
But trauma disrupts this flow.
The system gets stuck—either in hyperarousal (fight/flight) or hypoarousal (freeze).
Even neutral cues (a facial expression, a tone of voice) can trigger the trauma response.
The ability to return to calmness and connection becomes impaired.
This explains why trauma survivors may feel “on edge” all the time or completely disconnected without understanding why.
The Path to Healing: Reclaiming Safety and Regulation

The goal of trauma recovery isn’t to never feel fear, sadness, or anger again. Those are normal human emotions. Rather, it’s about building the capacity to return to safety—to return to the ventral vagal state where healing becomes possible.
Healing Strategies Include:
1. Body-Based Therapies
Talk therapy is valuable, but trauma is also stored in the body. Healing must include somatic approaches such as:
- Somatic Experiencing (SE)
- EMDR (Eye Movement Desensitization and Reprocessing)
- Polyvagal-Informed Therapy
2. Grounding Techniques
To anchor yourself in the present moment:
- Deep, slow breathing
- Mindfulness practices
- Body scans
- Holding ice, touching textures, or naming five things you see/hear/sense
3. Co-regulation
Connection heals. Safe relationships allow our nervous systems to attune and regulate.
- Being truly seen and heard
- Feeling emotionally safe with others
- Gentle physical presence (e.g., hugs or hand-holding, when welcomed)
4. Rhythmic Movement
Repetitive, rhythmic activities support nervous system regulation:
- Walking
- Drumming
- Dancing
- Rocking
5. Gradual Exposure with Support
Avoiding all triggers is not the solution. With the help of a therapist, gentle exposure can help reduce sensitivity and rebuild resilience.
You Are Not Broken—You Are Wired for Survival
If you or someone you love has gone through trauma, remember this: your reactions are not signs of being “weak” or “damaged.” They are signs that your nervous system is doing its best to protect you, even now.
Understanding the Polyvagal Theory can help trauma survivors—and their loved ones—make sense of confusing emotions and physical sensations. It removes shame and replaces it with insight and compassion.
Healing doesn’t happen overnight. But it’s absolutely possible—with time, support, and the right tools.
Final Thoughts
If you’ve experienced trauma, permit yourself to rest, to seek help, and to feel. Your body is not your enemy—it’s your ally, doing what it was built to do: survive.
The goal isn’t perfection. The goal is safety, regulation, and connection.
Take one step today. Maybe that step is learning more. Maybe it’s breathing deeply for 30 seconds. Maybe it’s reaching out for therapy.
Whatever it is, it matters.
You’re not alone—and you’re not broken.


Leave a comment